Implement a sustainable revenue management approach to AN-ACC using Mirus Metrics
ACFI was a transactional process which focused on growing top line revenue through the prompt identification and submission of claims. It was defined by mandatory and voluntary claiming activities whereby providers conducted their own assessments and processes were mainly in-sourced and decentralised.
Under AN-ACC, providers will need to consider the impact each admission, discharge, and/or reclassification will have on their workforce availability and care minute requirements. They may have to consider reducing care minutes through reclassifying re-abled residents, or request reclassifications to improve EBIT performance base on their contracted hours. To achieve this, the process can be split into two core activities:
- Step 1: AN-ACC forecasting and validation – is an analytical step to ensure accurate data to use for decision making.
- Step 2: Business scenario planning – is a business control step to determine reclassification scenarios to ensure minimal funding loss while maintaining care minute compliance.
Mirus Metrics enables both core activities to be managed, monitored, and measured.
Step 1: AN-ACC forecasting and validation
Complete an accurate AN-ACC data set to forward plan rostering operations.
Use the Mobile Assessment App exclusive to Mirus Metrics to replicate the external assessment process
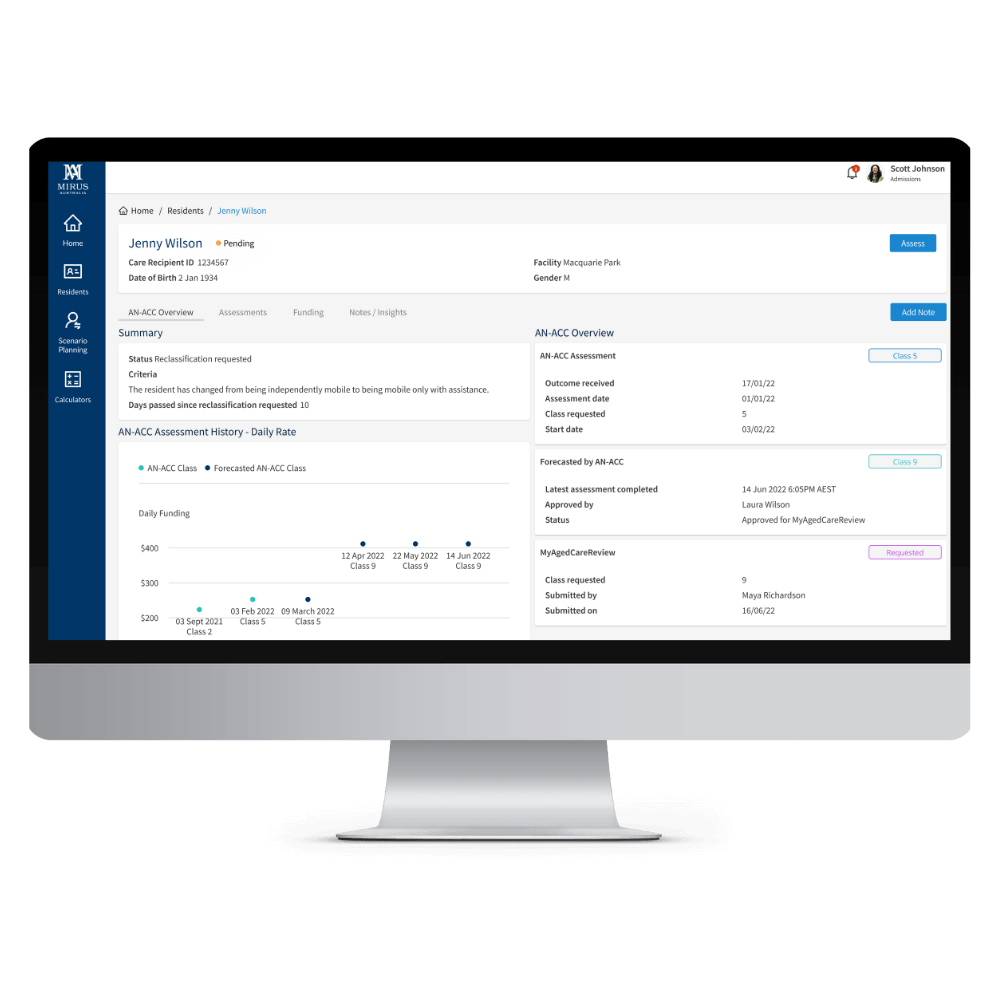
Use AN-ACC assessment inputs to accurately determine a forecasted AN-ACC classification, and track historical and active assessments assigned through Medicare.
Monitor the status of your reclassification requests, pending class outcomes and key performance data against your AMOs such as duration of time between reclassification request.
Manage resident movements, entries and leave through the Mirus Metrics application to keep your data relevant and timely ensuring your forward planning is accurately informed.
Step 2: Scenario planning
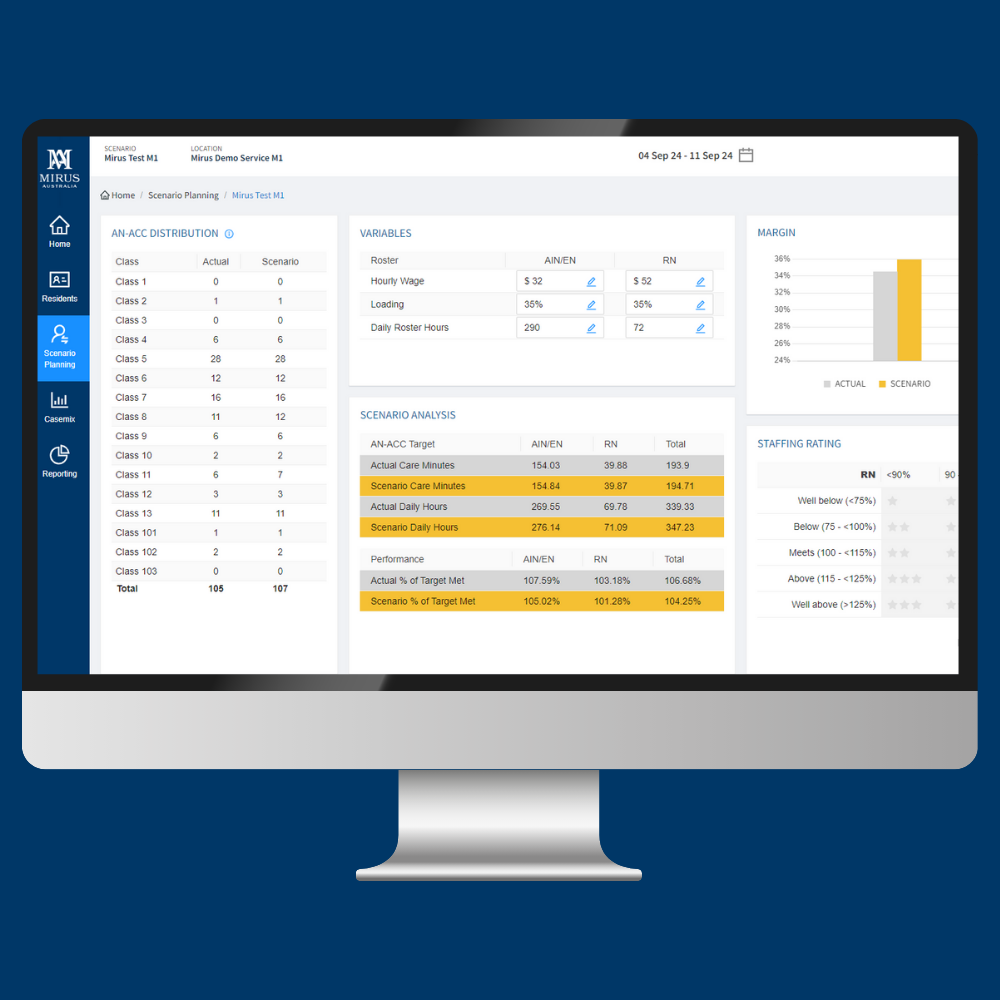
This innovative tool enables you to model the impact of potential reclassifications and admissions based on forecasted AN-ACC classifications.
Use the ‘Pre Admission’ feature to add new residents to the scenario.
Use the ‘Resident Forecast’ feature to categorise residents into three groups:
• Those with no changes
• Those who may move to higher subsidies and care minute requirements
• Those who may move to lower ones
By incorporating these forecasts into your planning, you can instantly assess the impact on funding, operational margin, and care minute compliance.
Connect Mirus Metrics structured data to your BI
The structured data features of Medicare and your assessment data within Mirus Metrics can be connected to your own internal BI tools. Mirus Metrics structured data can be adapted to your individual needs by using our ‘data as a service’ (DaaS) for your internal operations, industry benchmarking, Power BI dashboards and more with an API to your data warehouse.
Care Minutes dashboard

The Care Minutes dashboard allows you to view how current resident claims compare to the quarterly compliance target on a daily basis. This dashboard is essential for identifying unfunded care time and assessing the impact of AN-ACC claims on the next quarter’s target.
100+
Aged care organisations using Mirus Metrics
80,000+
Beds managed with Mirus Metrics
$5,600,000,000+
In Revenue under management with Mirus Metrics
Mirus Metrics is the only AN-ACC funding application software that brings together aged care funding data, industry data and forecasting insights into one easy-to-navigate solution.
With Mirus Metrics, you can:
- Manage and monitor your assigned AN-ACC classes as well as pending reclassifications requests.
- Assign AN-ACC forecasts to any resident and pre-admission prospect for data completeness.
- Upload key source evidence documents (AN-ACC Pack) and funding assessment notes to support the alignment of your forecasted class to the outcome determined by the Independent Assessment Process.
- Access key performance indicators to enable a measure of success.
- Build case mix performance scenarios ahead of planned rostering releases with both Active and Forecasted AN-ACC classes.
- Make your own AN-ACC assessment data through our Mirus AN-ACC application.
- Compare your facility KPIs, AN-ACC assessment input data, and AMO review trends with data from our industry segment.
Contact us today to learn more
Mirus Metrics FAQ
How will I monitor our care minutes in Mirus Metrics?
Care minutes requirements come from assigned AN-ACC classes. Mirus Metrics provides you with a view at any given time of your assigned active classes from the Department of Health and Aged Care. You can also assign forecasted AN-ACC classes against pending classifications. By assigning forecasted classifications within Mirus Metrics, you can track, and cost roster scenarios based on those AN-ACC classes.
How can I understand my performance compared to the industry?
One of our best-known features is the ability to view your organisation against the industry. Our benchmarking feature provides performance measures such as Average Daily Subsidy, and care minute averages by staff type etc, as well as across all segments which the industry is accustomed to.
Our new AN-ACC algorithm within Mirus Metrics will report industry trends based on the clinical indicators which are comprised of the assessment inputs of the AN-ACC. Items such as residents presenting with compounding factors, unplanned weight loss of 10% or more, as well as all other AN-ACC inputs which the Safety and Quality Commission now have access to via the Department of Health and Aged Care.
Are you connected with Services Australia?
Mirus Australia is the only software provider with Services Australia web services ready software across all aspects of aged care.
What do I need to know about data security?
We are ISO27001 ready and uphold compliance to the Aged Care Act, Data Security Act, and the Data Privacy Act.
Does Mirus Metrics integrate with other systems?
We have a suite of APIs that make integration with Mirus Metrics simple.
How can I train my staff?
Our dedicated support team is dedicated to ensuring a smooth onboarding process, training, and ongoing customer service. If your team need wider AN-ACC training, check out our Mirus Academy AN-ACC programs.