What you need to know for rostering AN-ACC minimum care minutes
June 16, 2022 | AN-ACC
By Grant Lewis, Senior Business Development Consultant
From October 2022, providers will need to start reporting whether they are meeting or exceeding their minimum AN-ACC care minute targets. Over the next couple of years, the new governments election promises will also kick in. The key dates are as follows:
- 1 Oct 2022 200 mins and 40 mins RN – Star Rating
- 1 Oct 2023 Mandatory 200/40 mins
- 1 July 2023 24/7 RN
- 1 Oct 2024 Mandatory 215 mins and 44 mins RN
Derived from their AN-ACC case mix, although the target will be set quarterly, the care minute number will fluctuate as frequently as daily depending on new admissions, departures, and resident reclassifications. This will mean that watching your care minutes change will be an important part of predicting your future workforce demands.
Through our work transitioning aged care clients from ACFI to AN-ACC, we field lots of questions related to care minutes and rostering. In this article, we’ve outlined three key considerations providers will need to adapt to by October this year. We have also provided some frequently asked questions and our answers at the end of this article.
1. AN-ACC will require you to plan how you will meet care minute requirements in advance
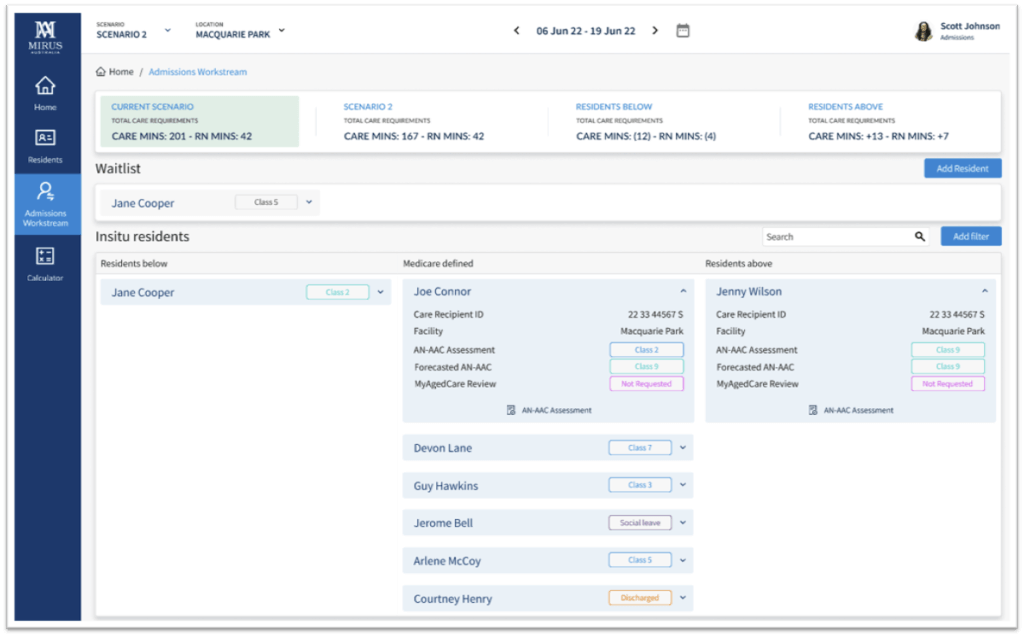
Providers should be thinking about how they ensure they will meet their care minute requirements in advance of a roster period as well as tracking it in real-time. There are three words that every aged care provider needs to familiarise themselves with: Integrated Data Model (IDM).
Rostering Coordinators will need to have access to Medicare, admissions and rostering data to allow them to effectively plan and manage a roster. These data outputs need to cover new admissions, potential discharges and residents identified for reclassification. To ensure best practice, these should consolidate into a single view so Rostering Coordinators can understand the impact on care minutes in real-time. This is the Integrated Data Model.
This “predictive” rostering approach allows the Roster Coordinator to build future rosters based on the predicted AN-ACC case mix and occupancy for that fortnight.
Click on image to expand
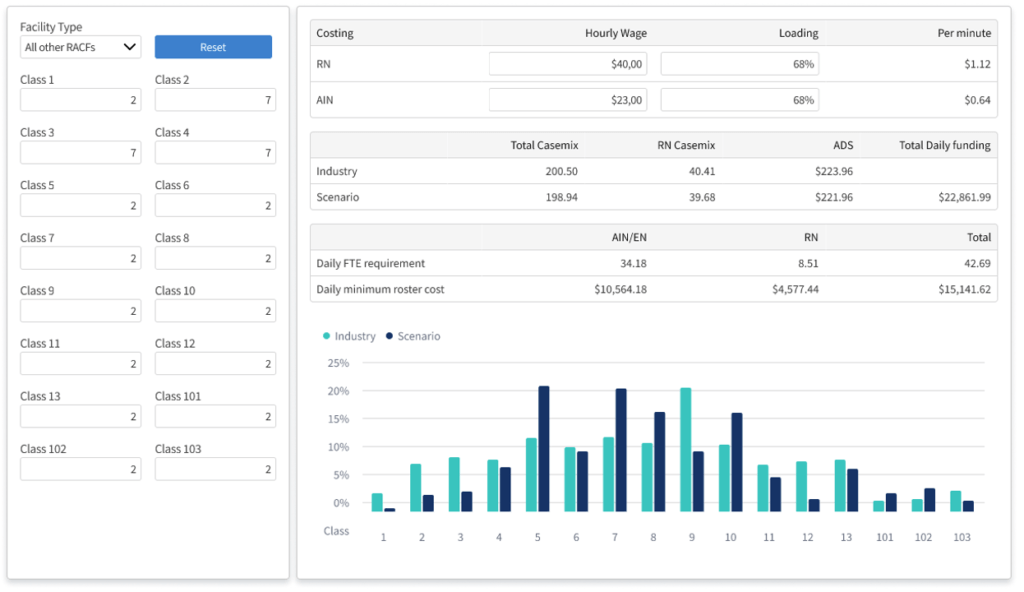
How a 7 minute minimum care time change will affect your roster
For the average sized facility in Australia, a change of just 7 minutes would result in having to increase or decrease hours by one FTE.
Consider the following scenario:
- If a facility with a care minute target of 200 minutes admitted 2 residents at Class 4, their new care minute target would be 198 minutes.
- Then if 4 residents AN-ACC classifications changed due to small changes in care needs (say, Class 8 to 6 and 10 to 5), this target could change again to 194 minutes.
- Finally, a further 2 residents at Class 11 are discharged, this could decrease again to 193 minutes
Now, this 7 minute swing is not likely to be as linear and certainly not all on the same day, but it is a likely scenario spread over a roster period. This means real-time data is critical to show how changes to the resident cohort affect minimum care minute requirements day by day.
Broadly speaking, this can be achieved by planning for different scenarios based on current and predicted case mix. These can then be tweaked due to departures or other unplanned events, but Rostering Coordinators need the tools to allow them to do this. For example, with the right insight, you could choose not to replace a sick shift, extended a shift, or add an entire shift to the roster to balance care minutes.
Access to this data in real-time is what ensures you are meeting your staff rating targets, maintaining compliance and that your costs don’t far exceed your revenue. The cumulative achievement of your quarterly target will be managed in the same way so that the anxiety is removed from your end of quarterly financial reporting (QFR). The rolling predictability of the data will ensure that future rosters are already planned before your quarterly target is even set.
Click on image to expand
2. Developing roster scenarios based on occupancy and case mix
Traditional rostering practices won’t address the agile environment that AN-ACC and minimum care minutes have introduced. Providers typically work with a master roster and a live roster, rolling forward the same base roster each period with changes that account for leave and unavailability.
However, this approach doesn’t allow for fluctuating care minute requirements, changing occupancy, or resident acuity. Your team needs the ability to quickly deploy a role-based roster template for any variety of operational scenarios you may come across over a 12 month period. This approach allows you to plan for whichever environment the facility finds themselves in at the time.
One option is to keep your hours as stable as possible by managing admissions and reclassifications but this may not always be possible so you will still need templates that cover a variety of scenarios you may be faced with. For example,
- 85% Occupancy + 210 minutes prpd (per resident per day)
- 85% Occupancy + 215 minutes prpd
- 85% Occupancy + 220 minutes prpd
- 95% Occupancy + 210 minutes prpd
- 95% Occupancy + 215 minutes prpd
- 95% Occupancy + 220 minutes prpd
- Outbreak template
3. Agency time and attendance hours need to be captured in the rostering system in real time
With ongoing staff shortages across the sector, another important factor to include in care time calculations is agency hours. Most rostering systems don’t allow time and attendance data to be captured for agency staff. We find clients receive an invoice from their agencies at the end of month with long arduous processes of reconciling the invoice to hours worked then add the hours in manually. AN-ACC’s introduction sees a need to have all hours worked and documented in real-time to understand if you are meeting your requirement on the same day as it’s being worked, this includes agency hours. Without including agency hours in your live roster, you will have no visibility of whether you have met or missed the requirement for the day or if you have significantly overspent. Under AN-ACC, the minimum care minute is prescribed so a key way to affect profitability is to manage the cost of each care minute. This can be done through staff mix (for different acuity mixes) and by minimizing expensive staffing alternatives (like agency).
FAQs
Why do I need to worry about care minutes now when it’s not required until October 2023?
Whilst compliance will be mandatory by October 2023, the star rating system is set to be rolled out from the end of 2022. This will allow consumers to see how your organisation compares to other competitors in meeting care minute targets. The quality agency will also have access to the star rating data and may pay extra visits to sites that are.
How regularly do I need to report my minutes?
Quarterly. However, your internal reporting should be able to track this daily so there are no surprises at the end of the quarter.
Should my rostering system report on worked hours each quarter?
Yes, your rostering system should be able to report on them. This will become a fundamental function of any rostering system. If not native functionality of your current platform, you will need to look at other platforms or consider ancillary processes and systems to report on this data.
What functionality should I be looking for in a rostering system?
- Does my roster have access to Medicare (the source of truth) for what my daily minimum care minutes need to be?
- Can it create multiple roster templates for various scenarios to address my care minute requirement at the time?
- Do I have sight of total worked hours in real-time including agency staff?
- Can I mark certain shifts with percentage weighting of direct care vs non direct care?
To find out how Mirus is addressing these issues with our rostering system, Mirus Works, contact us and one of our team members will be in touch.