Key Insights – A New Model for Regulating Aged Care
October 5, 2023 | Aged Care Reform

By Taranjot Minhas, Senior Consultant
With ongoing consultation on the regulatory model for aged care, the Department of Health and Aged Care conducted a webinar on the design of the new model in May (see recording here). As we progress towards the go-live date in July 2024, we are putting together a summary of the key concepts and insights from the consultation and documents so far, to help you prepare for what’s coming.
Overview
The new regulatory model will support planned reforms to in-home aged care and responds directly to Royal Commission’s recommendations, including:
- Recommendations 92 and 93 (provider approval and accreditation)
- Recommendations 13,14, 50, 131, 123, 133 and 135 (provider registration and obligations)
- Recommendations 97, 101, 102, 103, 134 and 136 (monitoring and enforcement) and
- Recommendations 10, 98 and 99 (complaints and whistle-blower protections).
Once finalised, the new model will be included in the New Aged Care Act and its supporting legislation. Under the new model, regulation will be proportionate to risk and support continuous improvement in the sector. The new model’s four foundations build an approach that is:
- Rights-based
- Person-centred
- Risk-proportionate and
- Focused on continuous improvement.
Raising the quality of aged care
To deliver consistent, high-quality care to older people, the model will:
- Drive cultural change across the sector
- Adopt relationship-based regulation to build:
- Stronger working relationships
- Deeper trust and
- more transparency in the sector.
This means, providers will be incentivised to improve, but there will be escalating enforcement actions available to the Regulator too. Providers that do not respect older people’s rights, fail to improve, or deliver high quality care, and put people at risk of harm will face strong enforcement action from the Regulator.
Figure 1 below shows the four “safeguards” – the range of regulatory tools and functions that will be used to help achieve these goals:
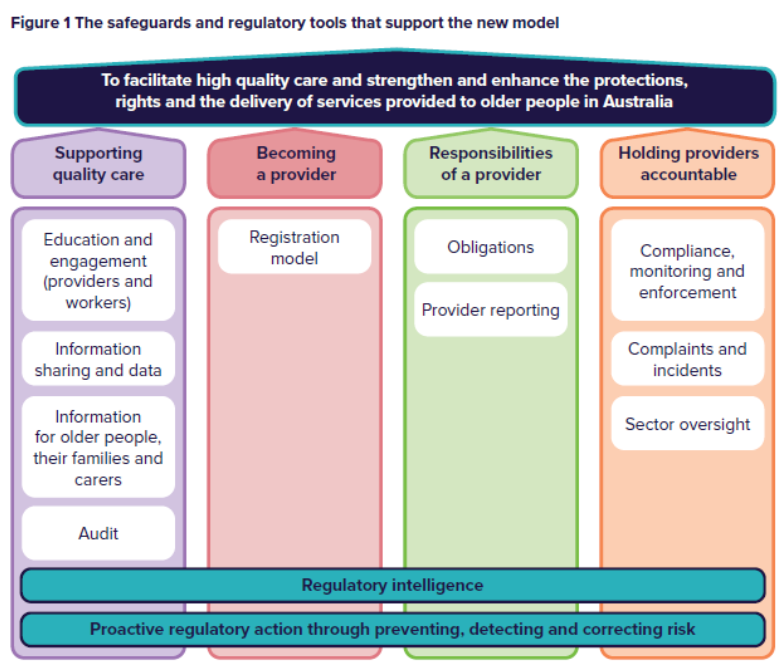
Below is a summary of the key concepts from each safeguard.
1. Supporting quality care
This safeguard places greater emphasis on relational regulation that aims to help drive cultural change and improve quality care outcomes for older people – aims to create a responsive and collaborative environment for providers to engage with the Regulator (and the Department) on innovation and continuous improvement, and to seek support and advice to avoid non-compliance with their responsibilities.
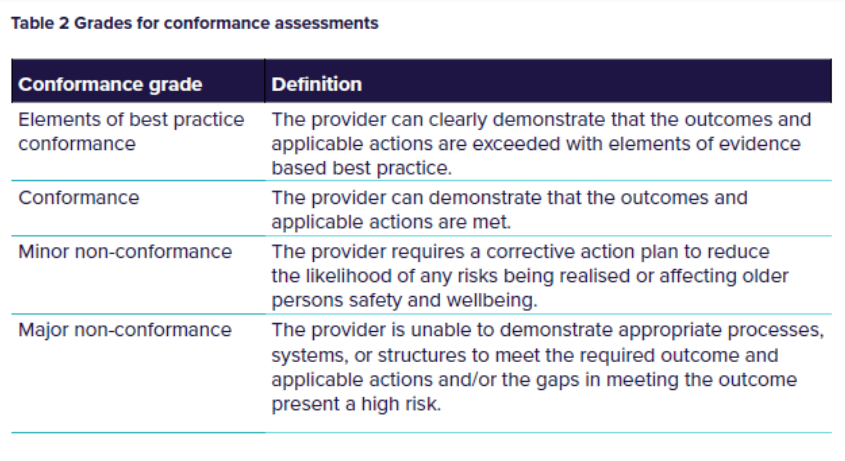
One of the major changes will be to audits against the Quality Standards, including graded assessment against the strengthened Quality Standards, which will incentivise providers to continuously improve and strive for excellence.
The outcomes of audits will support providers to:
- Share their plans for continuous improvement with older people and their representatives.
- Work with their consumer and quality advisory bodies to implement and sustain these improvements over time.
Incentivising high quality care will include several approaches, including:
- Publishing performance reporting for greater transparency and motivation to continuously improve.
- Promoting good performance, celebrating success within the sector, and enhancing public trust through commendations, endorsements from other bodies, communities of practice, titling, and promotion on Regulator website and My Aged Care.
- Graded assessments in the new audit process.
- Applying right-touch regulation to high performers such as changing evidence requirements for next registration cycle.
2. Becoming a provider
Universal provider registration and re-registration is proposed to replace the current ‘Approved Provider’ arrangements under the existing Act.
- To apply to all providers delivering Commonwealth subsidised aged care services.
- Propose to allow non-corporations e.g., sole traders and partnerships to register to deliver in-home aged care services.
- Six registration categories proposed, grouping services based on common characteristics, the associated service risks and the provider obligations to address the risks.
- Providers to register into one or more categories, to deliver a subset or all of the services within each category.
The proposed six registration categories are shown below:
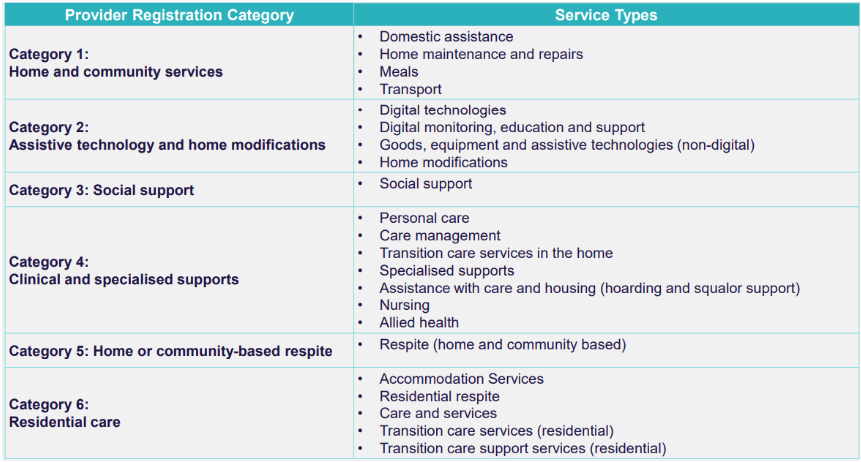
Table 2 below shows the grades for conformance assessments under the new audit process:
3. Responsibilities of a provider
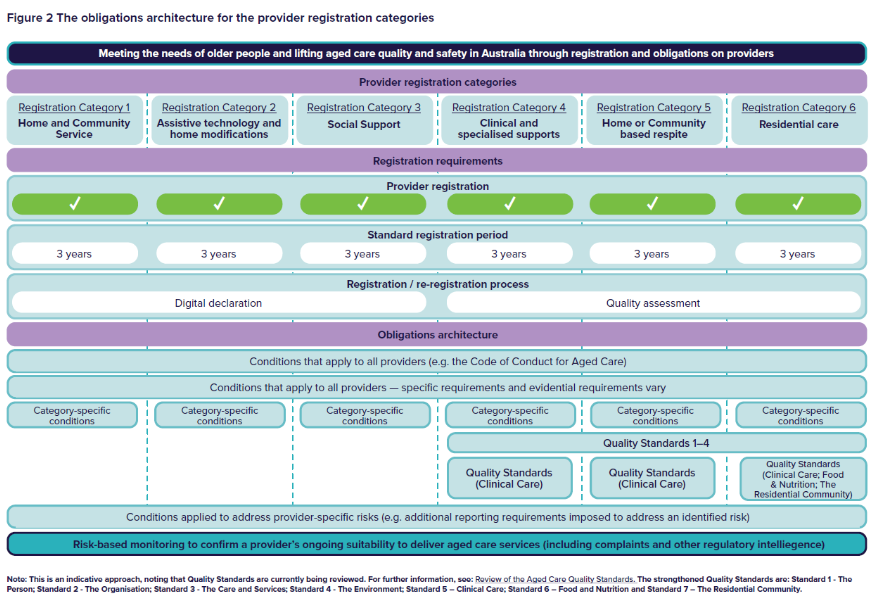
Provider responsibilities will be known as obligations in the new model. It is proposed that provider obligations in the new model be broadly grouped by:
- Overarching obligations that all providers must comply with regardless of conditions of registration.
- Core conditions of registration that apply to all providers regardless of the services being delivered, with evidence requirements and implementation of some conditions differing based on the registration category.
- Category-specific conditions of registration that apply to some providers based on their registration category.
- Provider-specific conditions of registration which are determined by the Regulator to manage risks associated with specific providers.
Figure 2 below shows the proposed approach and demonstrates how the registration categories and obligations are linked to enable risk-proportionate regulation.
4. Holding providers accountable
The rights foundation for the new Act will ensure that the protection and promotion of the rights of older people is central to the new aged care system. Older people will be encouraged and empowered to exercise their rights. They will also have pathways under the new Act to seek for their rights to be upheld.
Where the Regulator considers a provider or service to be a high risk to older people, they will be prioritised for risk-based monitoring. Risk-based monitoring by data and regulatory intelligence will signal a risk or issue that needs additional monitoring and/or a response. Monitoring could be site based, desk based, announced, or unannounced.
Changes are also being made to the Department and the Regulator’s systems to:
- Better enable them to detect and respond to issues including systemic issues and
- enable appropriate information sharing, including where complaints related to worker performance flow through to worker screening units (either in the NDIS or in aged care once established).
Enhanced complaints and feedback mechanisms will also translate into:
- Building a culture that values feedback and complaints
- Safe, accessible, and culturally appropriate pathways to provide feedback and raise complaints
- Restorative justice processes
- New powers to protect complainants from reprisals and
- Whistle-blower protections
Transitioning to the new model
It is proposed there will be a single ‘go-live’ commencement date, where the existing regulatory framework ceases and the new model commences. Existing providers of Commonwealth funded aged care programs will be deemed registered into relevant categories. While standard registration periods are expected to be 3 years, to avoid all providers having to re-register at the same time, re-registration timeframes for deemed providers will be staggered. Transition arrangements will also be made to ensure continuity of care for older people and minimise impact on providers.
The Department are now considering and analysing all feedback and will release a consultation report outlining what was heard during Stage 3 consultations.
Here are some helpful links for you to learn more:
- A new model for regulating aged care – Consultation paper 2 – Details of the proposed new model
- Frequently Asked Questions on a new model for regulating aged care – Consultation Paper No.2: Details of the proposed new model.
So, what do all these changes mean for your organisation? And how are you preparing for the new regulatory model?
For a tailored conversation around your organisation/facility, contact us.


