The AN-ACC case mix classification will impact your care minutes – do you have the data?
December 9, 2021 | Aged Care Reform
By Grant Lewis, Senior Business Development Consultant
The introduction of AN-ACC is fast approaching with the October 1st 2022 start date just around the corner. As an industry, we are still playing catch up on what it means for us and are yet to fully recognise that this will be the biggest shake up to Aged Care operations the industry has ever seen.
Both RCS and the soon to be incumbent ACFI operated independently from the rostering and admissions functions. AN-ACC will directly link the three, with each change in AN-ACC, along with admissions and departures, changing the minimum care minutes a facility will need to deliver.
Every facility will have its own unique target operating model (TOM) that will yield the best financial results and allow them to deliver the best care for their residents, although all three functions must work together to meet the TOM. This will see a greater reliance on real time data insights to run a sustainable operation.
The Old World – revenue, admissions and rostering act independently of each other
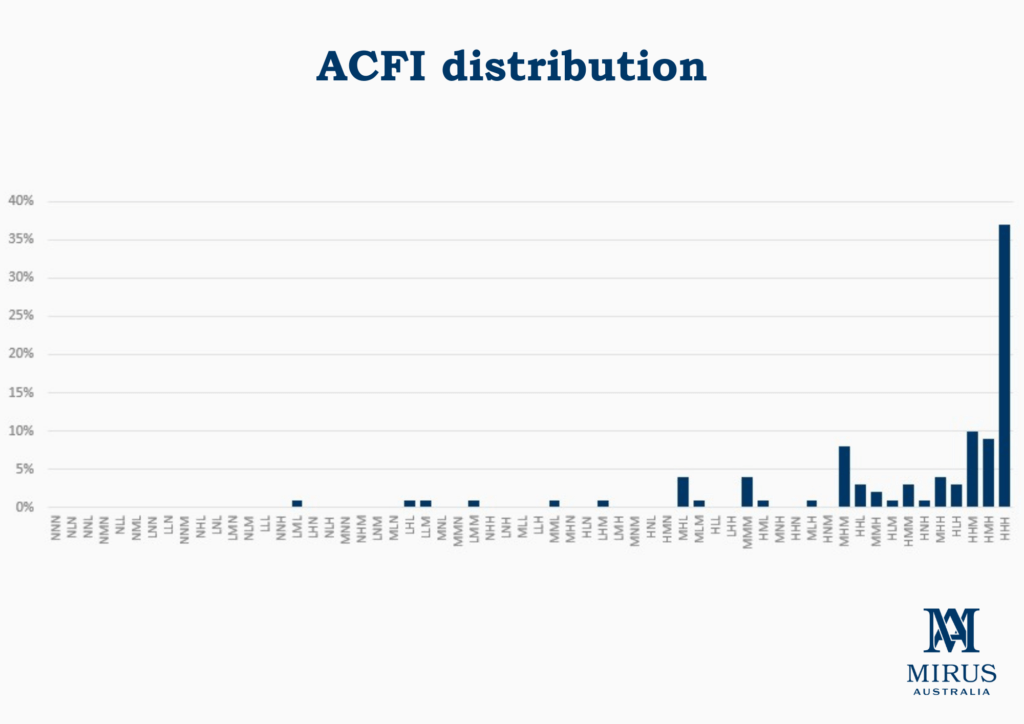
ACFI incentivised providers to optimize every resident’s ACFI claim and retain that claim even if care requirements reduced. Of the 64 ACFI classifications, over 55% of residents are classified in the top three highest ACFI categories (HHH, HMH, HHM). This distribution demonstrates that the model is no longer fit for purpose, thus the introduction of AN-ACC.
Click on image for full size
Industry occupancy is at an all-time low of 88.9% largely due to Home Care expansion, ACAR infrastructure ramp-up and compounded by COVID-19 restrictions in Australia’s two largest states – NSW and VIC.
The value created by the admissions function is three-fold:
- Increase occupancy to boost accommodation revenue.
- Admit residents that align with the RAC capital structure (heavy RAD payers or high volume of concessional residents).
- Only admit residents whose predicted ACFI won’t severely affect the Average Daily Subsidy (ADS) of the RAC.
In the new world, admissions teams will need to be aware of what AN-ACC classification their new entries are likely to be, as well as what pending AN-ACC classification changes to existing residents are in the waitlist.
Rostering is our opportunity to manage a facility’s biggest cost – staff wages.
Ordinarily this involves staff working off a master roster and filling shifts when required to cover things like annual and sick leave without going straight to agency or paying inflated casual rates. Many providers are using the same roster they have been using for years despite their fluctuating occupancy and/or average resident acuity changing.
The introduction of the 200 direct care minutes sees this change the rostering reliance on both the AN-ACC revenue and admissions function to allow stability in the roster. The 200 care minutes are only an average for the industry. Facilities with lower resident acuity will have a lower care minute requirement, while facilities with higher AN-ACC case mix will be required to deliver more than 200 minutes per day.
Click on image for full size
The New World – a target operating model centered around star ratings
Each facility will need to have their own unique target operating model which revolves around which star rating they want to maintain without the cost of their minimum care minutes exceeding the cost of the revenue their AN-ACC case mix is generating.
Rostering without the ability to have a daily view of upcoming AN-ACC reclassifications and new admissions waitlist AN-ACC estimates will result in significant overspend, and or damage to their star-rating.
Click on image for full size
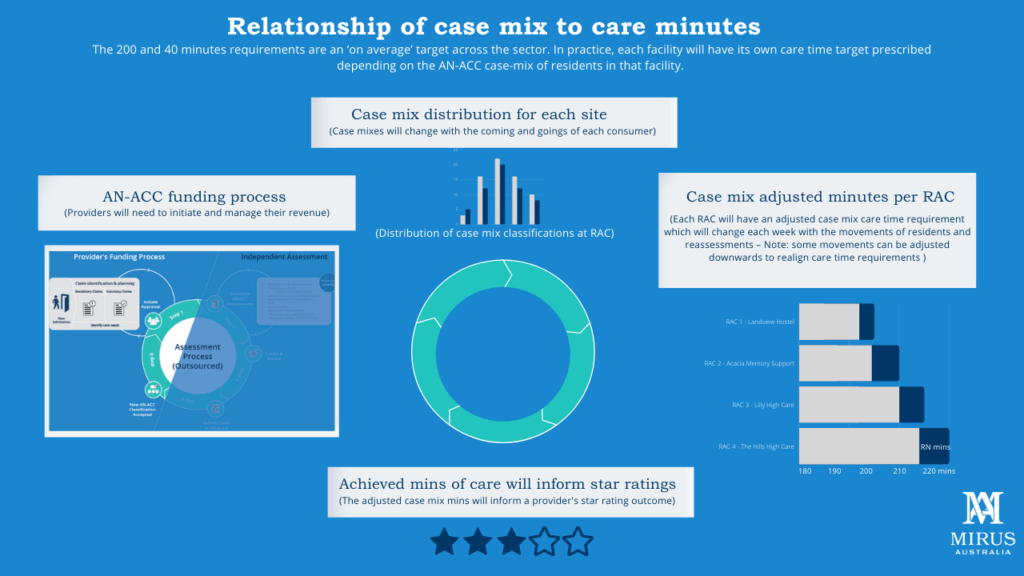
To avoid this, a regular data transfer will need to occur between rostering, revenue, and admissions. Previously, ACFI teams would uplift as many residents as possible, as soon as possible. Moving forward they may bank up a pool of potential classification changes but not ask for a reclassification change as the increases may result in an increase to the minimum care minutes of which the cost may exceed the additional revenue. Instead, they would need to wait until a lower funded resident enters the facility before lodging a reassessment or wait until a resident with a high AN-ACC classification departs the facility before making the request.
Regular strategic decisions will need to be made around how much a facility is willing to increase or decrease their minimum care minutes based on what star rating they want to maintain, the acuity of residents in the waitlist, and the list of residents awaiting reclassification. The traditional aged care mindset of a ‘set and forget’ master roster is now an antiquated approach. Providers will need to adopt a scenario demand approach where they can accurately forecast changes to AN-ACC case mix classification and upcoming new entries and how that will affect their upcoming rosters ahead of time.
To discuss this further, please feel free to contact me at grant.lewis@mirus.group or 0435 699 695.
Talk to us about your case mix today
Let’s talk about how your business could benefit,
starting with a free strategy session.
Further resources:
Mirus Works! – rostering software that works
Mirus AN-ACC Essentials training
Mirus ACFI and AN-ACC calculator
Mirus ACFI to AN-ACC Pathway (MAAP), a diagnostic to map your transition progress


